Wondering how to use an AI tool to address medical coding challenges? Healthcare industry leaders and RCM billing companies have been looking for a medical coding solution for a long time now. In the ever-evolving landscape of healthcare, precision, and accuracy in medical coding are critical for billing, compliance, and overall patient care. Traditional manual coding processes are not only time-consuming but also prone to errors, leading to financial losses and potential compliance issues. This article walks you through how to use AI for medical coding and elaborates on the transformative role of AI tools in improving medical coding accuracy, providing healthcare professionals and RCM billing companies with efficient solutions for the challenges they face.
- Understand the Importance of Medical Coding Accuracy
Medical coding is not a simple task where any layperson can analyze the clinical encounters and translate them into billable code. It requires certified coding professionals with vast experience and knowledge. The medical codes act as a final statement of the patient’s encounter. Hence, medical coding accuracy is of vital importance.
The hardest part of medical coding is staying up-to-date with the changing payer rules and document requirements.
If medical codes are incorrect, it can lead to a range of consequences with significant implications for healthcare providers, patients, and the overall healthcare system. Here are some possible results:
a. Billing Errors and Revenue Loss: Incorrect medical codes can result in billing errors, leading to underbilling or overbilling for services rendered. This can result in financial losses for healthcare providers and impact the overall revenue cycle. It may also lead to disputes with insurance providers and delayed reimbursements.
b. Compliance Issues and Legal Consequences: Inaccurate medical coding can lead to non-compliance with healthcare regulations and coding guidelines. This poses legal risks and can result in audits, fines, or penalties. Healthcare providers must adhere to specific coding standards, and deviations may raise concerns about fraudulent activities or inadequate documentation.
c. Impacts on Patient Care: Incorrect medical codes can lead to misunderstandings in patient records, affecting the continuity and quality of care. Inaccurate coding may result in inappropriate treatment plans, medication errors, or inadequate follow-up care. Patient safety is compromised when the healthcare team relies on inaccurate information for decision-making.
e. Operational Inefficiencies: Healthcare organizations rely on accurate coding for efficient operations, resource allocation, and planning. Inaccurate codes can disrupt these processes, leading to inefficiencies, increased workload, and delayed decision-making. Operational workflows, such as claims processing and reporting, may be adversely affected.
f. Negative Impact on Reimbursements: Insurance companies often use medical codes to determine reimbursement amounts. Incorrect coding may result in lower reimbursements than deserved or lead to claim denials. This financial impact can strain the resources of healthcare providers and hinder their ability to provide quality care.
g. Reputation Damage: Inaccurate coding can harm the reputation of healthcare providers. Billing discrepancies, compliance issues, and legal consequences can erode trust among patients, insurers, and regulatory bodies. A tarnished reputation may lead to a loss of patients and business opportunities.
h. Audit and Corrective Measures: Healthcare organizations may face audits and corrective actions to rectify coding errors. This involves investing additional time and resources to review and correct discrepancies, leading to disruptions in daily operations and diverting attention away from patient care.
i. Increased Administrative Burden: Incorrect codes may necessitate additional administrative work to rectify billing errors, respond to audits, and address compliance issues. This increased administrative burden can strain the resources of healthcare providers and impact their ability to focus on core patient care activities.
In summary, the consequences of incorrect medical coding are multifaceted, affecting financial, legal, operational, and patient care aspects of healthcare delivery. Ensuring accurate coding is essential for maintaining the integrity of healthcare data, supporting optimal patient care, and sustaining the financial viability of healthcare organizations.
- The Role of AI in Enhancing Medical Coding Accuracy
Optimizing medical coding is crucial for preventing claims denials. Healthcare providers must adhere to payer requirements and use accurate codes for services provided during a clinical encounter.
Healthcare facilities have slowly begun adopting artificial intelligence (AI) for all aspects of healthcare processes from documentation to patient care.
Identification of keywords:
-
- AI medical coding tools use machine learning algorithms to analyze vast amounts of healthcare data, identifying keywords in medical documentation.
- Recognition of keywords along with other information enables the system to suggest relevant codes based on historical data, improving efficiency and accuracy in code assignment.
Streamlining Code Assignment:
-
- The tool automates the process of assigning medical codes by analyzing patient records, diagnoses, and procedures.
- By streamlining code assignments, healthcare professionals can save time and reduce the likelihood of manual errors, leading to a more efficient coding workflow.
Reducing Clerical Errors:
-
- Automation minimizes the risk of clerical errors associated with manual coding processes.
- By automating repetitive tasks, AI tools enhance accuracy, ensuring that medical codes align with the documented information, reducing the potential for billing errors and compliance issues.
Natural Language Processing (NLP) in Medical Coding:
Natural Language Processing (NLP) integrates computational linguistics, machine learning, and deep learning techniques for the analysis of human language. Computational linguistics is the discipline that focuses on comprehending and creating models of human language using computers and software tools.
Parsing Unstructured Clinical Text:
-
- NLP enables AI tools to understand and process unstructured clinical text, such as physician notes and narratives.
- By parsing this unstructured data, the tool extracts key information relevant to medical coding, facilitating a more comprehensive and accurate coding process.
Extracting Relevant Information:
-
- NLP algorithms analyze clinical text to extract pertinent information, including diagnoses, procedures, and other crucial details.
- This extraction process ensures that the AI tool captures the nuances of the medical documentation, contributing to precise code suggestions.
Enhancing Specificity and Detail:
-
- NLP enhances the specificity and detail in medical coding by capturing context and relationships within the clinical text.
- The tool’s ability to understand the subtleties of language contributes to more accurate code recommendations, reducing ambiguity and improving the quality of coded information.
The tool is trained with the latest guidelines and data which allows it to refine its coding recommendations, reducing errors and enhancing overall accuracy as it encounters and processes more healthcare information.
Implementing and using an AI Tool in the Medical Coding Process
As the saying goes in 2024, AI won’t replace medical coders, but people skilled and experienced in using AI-driven medical coding tools will replace you.
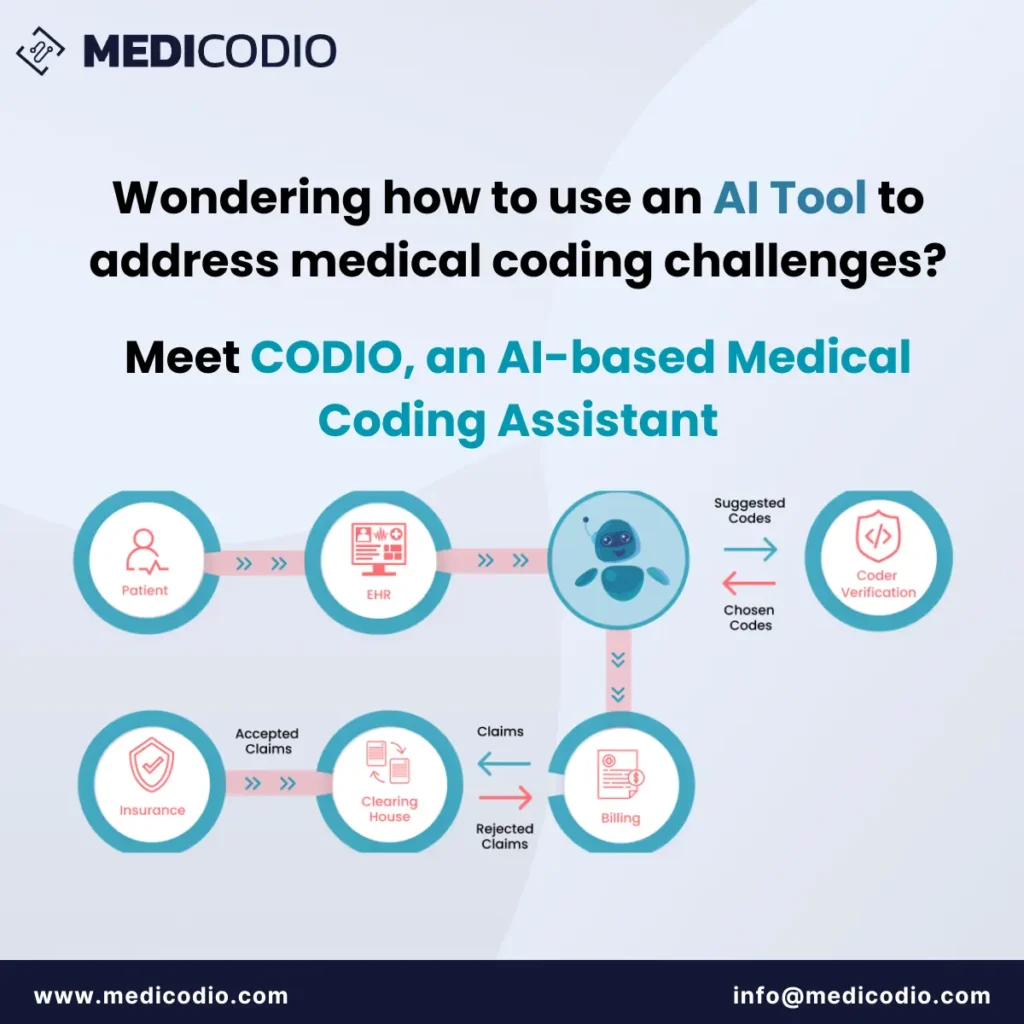
Once the tool is implemented and integrated with other tools, all that medical coders have to do is log in to the AI-powered medical coding platform and choose a particular patient’s medical record required to code.
The AI-medical coding platform will retrieve the patient’s information such as name, age, gender, and any relevant medical history from CRM. It will review the doctor’s notes, test results, and any other pertinent documents using advanced algorithms. The tool also suggests potential medical codes for diagnoses, procedures, and other relevant information based on the input data.
The coder then has to cross-reference the AI-generated codes with the patient’s records. Ensure accuracy by confirming that the codes align with the documented medical procedures and conditions.
Manual Adjustments (if necessary): Make any necessary manual adjustments to the codes if the AI suggestions need refinement. Your expertise is crucial in ensuring the final codes accurately represent the medical services provided.
Document any specific details or justifications for the chosen codes. This step is vital for transparent communication within the healthcare system.
Finalize and Submit: Once you are satisfied with the coded information, finalize the coding process. Submit the coded data to the billing department for further processing.
Review Feedback: Periodically review any feedback or updates from the AI tool. Stay informed about system enhancements or adjustments to improve your coding efficiency.
How to Choose the Right AI-based Medical Coding Software in 2024?
Choosing the right AI-based medical coding software is crucial for medical coding accuracy and efficiency in healthcare billing. Precise coding ensures proper reimbursement, reduces billing errors, and enhances compliance with regulatory standards. A reliable system streamlines the coding process, saving time and resources for medical coders. Moreover, accurate coding supports transparent communication among healthcare providers, insurers, and regulatory bodies, ultimately contributing to improved patient care and the financial health of healthcare organizations. In summary, the right AI-based medical coding software is essential for optimizing revenue cycles, maintaining compliance, and fostering a seamless and error-free billing workflow.
Make sure that you are working with a tool that has the most updated information. Medical coders have a crucial role to play in the healthcare industry. They need to stay up-to-date with the latest developments and changes in their field. Every year, updated ICD-10-CM and ICD-10-PCS code sets are released on October 1st, and updated CPT and HCPCS Level II code sets are released on January 1st. These updates include new codes, deleted codes, and revised code descriptions. Medical coders need to stay current with these changes to perform their tasks accurately.
How does CODIO, an AI-based medical coding tool streamline the medical coding process for its users?
-
- CODIO employs a combination of AI, Machine Learning (ML), Robotic Process Automation (RPA), and Natural Language Processing (NLP) to analyze patient charts and suggest relevant codes.
-
- Medical coders can then review these suggestions and select the most appropriate codes after verification, significantly enhancing their productivity.
-
- The tool is capable of reading electronic health records (EHRs), electronic medical records (EMRs), and physician’s notes, allowing for a wide range of data input methods.
Features, Functionalities, and Benefits: The CODIO Advantage
MediCodio’s CODIO offers a suite of features and functionalities that bring tangible benefits to the medical coding process.
-
- Intelligent Code Suggestions: By analyzing medical records, CODIO provides highly relevant code suggestions, streamlining the medical coder’s decision-making process.
-
- Expert Medical Coder Verification: A team of professional medical coders reviews the recommended codes to ensure top-notch accuracy and compliance.
-
- Efficiency and Time Savings: Medical coding becomes 45% faster with CODIO, allowing healthcare organizations to save on resources.
-
- Reduced Denial Claims: The accuracy of CODIO’s suggestions leads to fewer claim denials and a more robust revenue cycle.
-
- Increased Revenue: With the ability to handle more records with minimal errors, CODIO helps boost an organization’s revenue.
-
- Reduced Coder Burnout: By taking on the bulk of the coding process, CODIO mitigates the risk of burnout among medical coders.
Use Cases and Potential Applications: Broadening Horizons with CODIO
CODIO’s application isn’t limited to a single aspect of healthcare. Its use cases span across various functions and types of organizations in the medical field.
-
- Healthcare Facilities: CODIO can be used by hospitals and clinics to ensure that medical coding is done swiftly and accurately, which is critical for patient record keeping and insurance reimbursement.
-
- RCM Companies: For companies specializing in revenue cycle management, CODIO automates workflows and enhances the management of medical records, directly impacting their bottom line.
-
- Individual Medical Coders: Freelance or in-house medical coders can use CODIO to augment their expertise and handle a larger volume of work with greater precision.
Target Audience: Who Benefits from MediCodio’s Solutions?
MediCodio’s products are crafted with specific audiences in mind, each benefitting from the sophisticated AI-assisted medical coding that CODIO provides.
-
- Healthcare Facilities: Hospitals and clinics looking to improve their coding accuracy and efficiency.
-
- RCM Companies: Organizations that seek to optimize their revenue cycle and reduce claim denials.
-
- Medical Coders: Individual coders who aim to enhance their productivity and reduce the risk of burnout.
Conclusion
As the healthcare industry embraces digital transformation, leveraging AI tools to enhance medical coding accuracy is not just a choice but a necessity. The benefits go beyond financial gains, extending to improved patient care, compliance with regulations, and the overall efficiency of healthcare operations. By understanding the challenges, implementing AI solutions, and fostering a collaborative environment, healthcare professionals can navigate the evolving landscape and ensure accurate medical coding for the benefit of patients and the industry as a whole.