What do you think is more important for oncology practice to run seamlessly: Accurate coding or ethical billing strategies? Well, truth be told, both are equally important. However, according to various studies, it is reported that compared to any other specialty, oncology has more complicated denied claims which require an effective denial management solution.
In June 2022, Experian Health surveyed 200 revenue cycle decision-makers to shed light on the current claims environment. 30% of respondents say denial rates are increasing. 52% of the healthcare leaders are either replacing or upgrading previous claim processing technology.
One of the major reasons behind the increasing denial rate is inaccurate coding. Oncology coding is the base for oncology billing, the slightest error in the medical coding process will negatively impact the payment and revenue.
Oncology treatment is highly expensive. Hence, you must be ready to tackle the oncology claim denial problem head-on.
What’s Oncology medical coding and billing?
Oncology medical coding and billing is the process of analyzing patient’s medical records, assigning appropriate codes, and submitting claims to insurance companies or other payers for oncology-related billing services associated with cancer management. The process of successful oncology medical billing involves verifying patient coverage, documenting medical history accurately, submitting claims promptly, and ensuring compliance with regulations through a thorough understanding of medical coding.
Example of Oncology Codes
It is important to differentiate between current and previous cancer conditions based on physician documentation. Here are some examples of oncology coding:
Challenges in Oncology Medical Coding
These challenges stem from the complexity and ever-evolving nature of oncology practices, as well as the need for accurate and detailed coding for proper reimbursement and data analysis. Here are some key challenges in oncology coding:
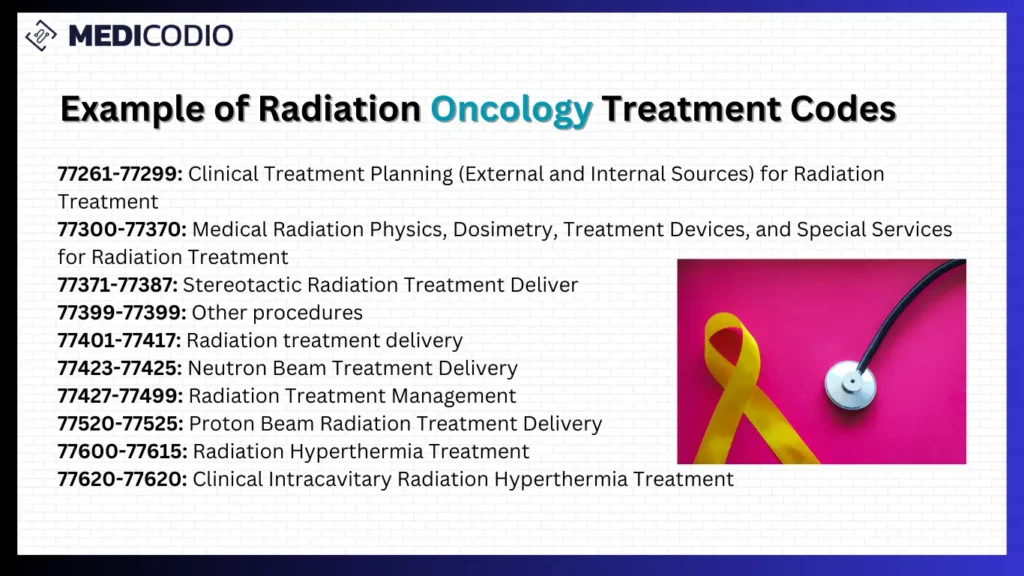
Complexity of Oncology Procedures: Oncology procedures often involve intricate surgeries, chemotherapy, radiation therapy, and other advanced treatments. Deciphering and accurately coding these complex procedures requires a deep understanding of medical terminology, anatomy, and various treatment modalities.
Frequent Updates to Coding Guidelines: Oncology coding guidelines are subject to frequent updates and changes. Keeping up with revisions from organizations like the American Medical Association (AMA) and Centers for Medicare & Medicaid Services (CMS) is crucial to ensure accurate coding and compliance.
Multiple Diagnoses and Co-Morbidities: Cancer patients frequently present with multiple diagnoses and co-morbidities, making it challenging to capture the full clinical picture. Accurate coding demands a comprehensive understanding of the disease process, its stages, and associated conditions.
Evolution of Treatment Modalities: Advances in oncology lead to the development of new treatment modalities and technologies. Coders must stay informed about these innovations to accurately code the procedures, ensuring proper reimbursement and reflecting the complexity of the provided care.
Documentation Variability: The quality and specificity of medical documentation can vary among healthcare providers. Incomplete or vague documentation can hinder accurate coding, potentially leading to coding errors, claim denials, and reimbursement issues.
Navigating Multiple Code Sets: Oncology coders must work with multiple code sets, including CPT (Current Procedural Terminology), ICD-10 (International Classification of Diseases, 10th Edition), and HCPCS (Healthcare Common Procedure Coding System). Balancing these code sets while ensuring proper code linkage is essential for accurate reimbursement.
Insurance Pre-authorization Challenges: Many oncology treatments require pre-authorization from insurance companies. Coders must be familiar with the specific coding requirements for pre-authorization and work closely with healthcare providers to ensure proper documentation is submitted to facilitate the approval process.
Coding for Clinical Trials: Oncology practices often participate in clinical trials, which may involve unique coding requirements. Coders must be knowledgeable about the specific coding rules and guidelines for reporting services related to clinical trial participation.
Billing and Reimbursement Issues: Oncology coders face challenges related to billing and reimbursement, such as ensuring proper use of modifiers, understanding bundling and unbundling rules, and navigating payer-specific coding requirements to avoid claim denials.
Tips to Prevent Oncology Claim Denials
How can a medical billing company mitigate claim denials?
Engaging a billing partner can assist oncologists in optimizing reimbursement and reducing claim denials by leveraging their specialized expertise in current coding and billing practices.
Billing companies provide a proficient team of Certified Professional Coders (CPC) and billers who adeptly address various challenges in oncology billing. Outsourcing eliminates the burden of recruiting or training staff on evolving oncology procedures, new codes, and coding modifications.
Coders within the billing team assign codes meticulously, ensuring prompt reimbursement without the need for additional training or system adjustments for ICD-10 implementation.
An experienced team manages underpayment issues, ensures timely claim submissions, conducts follow-ups and ensures compliance with HIPAA and other regulatory changes.
Even during holidays or staff leave, the billing partner takes charge of claims and oversees the entire revenue cycle management process.
Regular scrutiny and analysis of claims help identify reasons for denials, allowing for effective problem-solving. By deploying AI-based medical coding tools can also help in addressing concerns like time loss and reduced staff productivity.
In essence, partnering with an AI-powered medical coding software company offers a comprehensive solution to enhance revenue and streamline the coding and billing process for oncology practices.
AI-enabled technology can optimize claims management
As healthcare companies are experiencing an increase in claims denials, their bottom line is affected drastically. However, incorporating artificial intelligence (AI) can help providers minimize the impact of this issue by streamlining their claims management process and reducing denials.
MediCodio is a novel AI-based medical coding tool that can streamline the medical coding process by suggesting accurate codes. Our technology is engineered to minimize errors and maximize revenue, all while ensuring compliance and improving patient satisfaction.
The software continuously adapts to the ever-changing coding guidelines and supports all specialties. By providing 85% accuracy, the platform helps medical coders in the reduction of claims denials and enables healthcare providers to focus on high-priority claims, thereby boosting overall revenue.